- Description
- Reviews (0)
- Store Policies
- Inquiries
Description
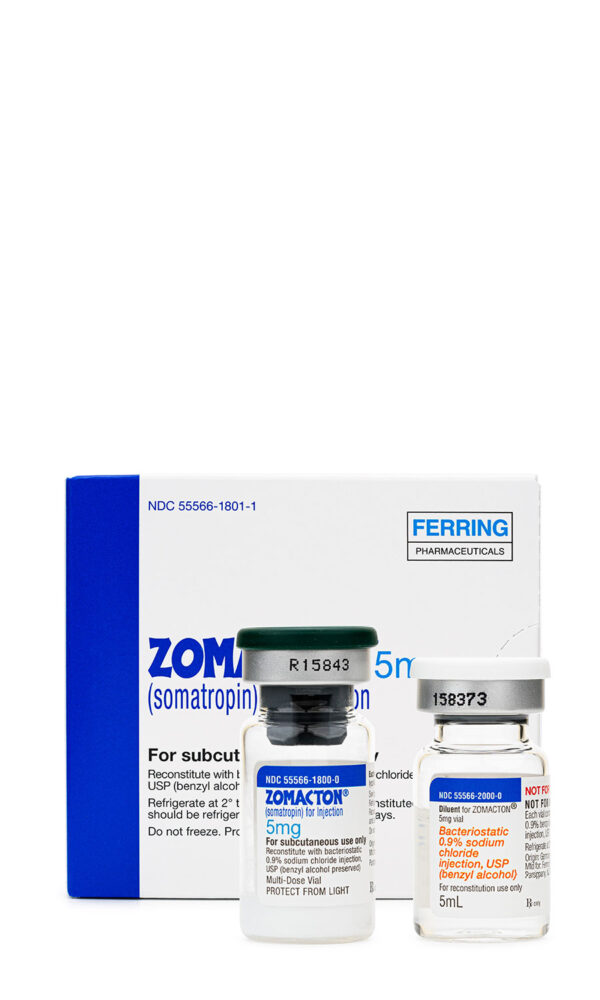
Dosage Strength of Zomacton Injection
5 mg Lyophilized Vial
Rh-GH, or Somatropin, is a pure form of recombinant growth hormone produced by either mammalian cells or Escherichia coli. The pituitary gland is where endogenous human growth hormone (hGH) is produced. In 1956, the first growth hormone was isolated, and its structure was identified in 1972. Growth hormone (GH) was previously generated from human cadavers prior to 1985; however, this practice was discontinued due to Creutzfeldt-Jakob virus contamination of the product. Somatropin is approved for use in adults with short bowel syndrome, growth hormone deficiency (GHD), growth failure, or short stature, as well as cachexia and AIDS wasting. In studies for the treatment of HIV-associated adipose redistribution syndrome (HARS), somatropin has been shown to reduce visceral adipose tissue, according to limited short-term data. Several somatropin products are available, all with varying indications and dosage regimens. Care should be taken in product selection as products may not be considered interchangeable. Somatropin was originally approved by the FDA in 1987.
In children and adolescents, endogenous growth hormone is in charge of stimulating healthy skeletal, connective tissue, muscle, and organ development. In adult metabolism, it also has a significant impact. All of these behaviors are mimicked in recombinant products. As it binds to growth hormone (GH) receptors, somatropin causes a number of physiological effects that can be divided into direct and indirect ones. The direct effects include the antagonistic activity of the peripheral action of insulin and the subsequent stimulation of insulin secretion; stimulation of the liver’s and other tissues’ somatomedin or insulin-like growth factor (IGF) production; stimulation of adipose tissue’s triglyceride hydrolysis; stimulation of the hepatic glucose output; induction of a positive calcium balance; and retention of sodium and potassium. These effects oppose the action of insulin on fat and carbohydrate metabolism and are potentiated by glucocorticoids.
The anabolic and growth-promoting actions of somatropin are indirectly mediated by somatomedins or insulin-like growth factors (IGFs). IGFs circulate around the body and attach to certain IGF receptors. IGF-1 and IGF-2 are the two known IGFs. Growth hormone appears to be primarily mediated by IGF-1, whereas IGF-2 has more insulin-like activity. The primary anabolic actions of IGFs include inducing cell proliferation and growth, stimulating amino acid transport, and stimulating DNA, RNA, and protein synthesis. IGF-1 is directly responsible of chondrogenesis, skeletal development, and soft tissue growth. By altering the cartilaginous growth regions of long bones, linear growth is encouraged. The quantity and size of skeletal muscle cells, the size of organs, and the activation of erythropoietin all contribute to the stimulation of growth. Growth hormone can affect the gut directly or indirectly through the systemic or local production of IGF. Growth hormone has been found to improve the transmucosal transfer of nutrients, electrolytes, and water in in-vivo experiments. Glucocorticoids prevent these indirect effects.
Injected intramuscularly or subcutaneously, somatropin reaches its peak plasma concentrations within 2 to 6 hours after administration. About 20% of the circulating somatropin is bound to growth hormone-binding protein. IGF-1 plasma concentration peaks occur roughly 20 hours following somatropin administration. The liver, kidney, and other tissues all metabolize somatropin. Somatropin receives glomerular filtration and the molecule is cleaved in the kidney. The peptides and amino acids are released back into the bloodstream after being cleaved in the renal cells. Urine excretion is not very common. The half-life of plasma elimination is 20 to 30 minutes. The serum concentrations decline with a half-life of roughly 3–5 hours as a result of the continuous release of somatropin from the intramuscular or subcutaneous location. The effects of somatropin extend considerably longer than its half-life of elimination due to the slow induction and clearance of IGF-1.
Route-Specific Pharmacokinetics:
Subcutaneous Route: Somatropin is first released from the microspheres via diffusion after subcutaneous injection of the depot formulation, and then it is released by both polymer degradation and diffusion. When compared to single dose Nutropin AQ and when compared to chronically dosed Protropin, the estimated bioavailability after a single dose of Nutropin Depot varies from 33 to 38% and 48 to 55%, respectively. Somatropin is thought to be distributed and removed in a similar way to somatropin designed for everyday use once it has been released and absorbed. Both the Cmax and AUC are proportional to the dose. After a single dose of 0.75 or 1.5 mg/kg, serum growth hormone levels remain over 1 mcg/l for 11–14 days.
Special Populations:
Pediatrics: It appears that the clearance of somatropin in children and adults is similar; however, no pharmacokinetic studies have been conducted in children with short bowel syndrome.
Gender Differences: Biomedical literature indicates males may clear somatropin more quickly than females, although no gender-based analysis is available.
For the treatment of growth hormone deficiency, growth failure, or short stature:
NOTE: The response to somatropin therapy in pediatric patients tends to decline with time. However, the failure to increase growth rate, especially during the first year of therapy, necessitates close assessment of compliance and evaluation for underlying causes of growth failure, such as hypothyroidism, undernutrition, advanced bone age, and antibodies to recombinant human growth hormone.
For replacement therapy in adults with growth hormone deficiency (GHD) for either childhood onset (secondary to congenital, genetic, acquired, or idiopathic causes) or adult onset (endogenous or associated with multiple hormone deficiencies, i.e., hypopituitarism, as a result of pituitary disease, hypothalamic disease, surgery, radiation therapy, or trauma):
NOTE: In general, the diagnosis of both adult or childhood onset growth hormone deficiency should be confirmed by an appropriate growth hormone stimulation test. Stimulation testing may not be necessary in patients with congenital/genetic growth hormone deficiency or multiple pituitary hormone deficiencies due to organic disease.
NOTE: Clinical response, side effects, and age- and gender-adjusted serum IGF-I levels may be used to guide dose titration. This approach will tend to result in larger doses for women compared to men, smaller doses for adult-onset GHD patients compared with childhood-onset GHD patients, and smaller doses for older and obese patients.
NOTE: Patients with childhood onset growth hormone deficiency whose epiphyses are closed should be reevaluated before continuation of somatropin therapy.
Geriatric: See adult dosage. Consider giving a lower starting dose and smaller dose increments to minimize adverse events.
Subcutaneous dosage: Adults: Initially, not more than 0.004 mg/kg SC per day. After 6 weeks, the dose may be increased, as tolerated, to a maximum of 0.016 mg/kg per day. Alternatively, the following non-weight based approach may be used: initially, 0.2 mg SC per day (0.15—0.30 mg SC per day); increase dose gradually by increments of approximately 0.1—0.2 mg/day every 1—2 months based on clinical response and serum insulin-like growth factor I (IGF-I) concentrations. Decrease the dose as necessary based on the adverse events and/or serum IGF-I concentrations above the age- and gender-specific normal range. Maintenance dosages vary considerably from person to person and between male and female patients. NOTE: Obese patients are more likely to experience adverse effects when dosed by weight.
Geriatric: See adult dosage. Consider giving a lower initial dose and smaller dose increments to minimize adverse events.
For the long-term treatment of growth failure in children who have growth hormone deficiency due to inadequate growth hormone secretion:
Subcutaneous dosage: Children: 0.024—0.034 mg/kg/dose SC given 6 to 7 times a week. Dosage should be individualized for each patient.
For growth failure due to Prader-Willi syndrome:
Subcutaneous dosage: NOTE: Genotropin or Omnitrope should only be used in Prader-Willi syndrome patients who have a diagnosis of growth hormone deficiency; Genotropin and Omnitrope are contraindicated in Prader-Willi syndrome patients who are severely obese or who have severe respiratory impairment.
Children: Generally, 0.24 mg/kg SC per week divided into 6 or 7 equal daily injections.
For the long-term treatment of growth failure in children born small for gestational age (SGA) who fail to manifest catch-up growth by age 2-4:
Subcutaneous dosage: Children: Up to 0.067 mg/kg/day SC (0.47 mg/kg/week) is recommended. Recent data suggest that for younger children with a baseline HSDS between -2 and -3, the initial dose is 0.033 mg/kg/day SC with upwards titration as needed. For children with a baseline HSDS < -3 or for older/prepubertal children, the recommended initial dose is 0.067 mg/kg/day SC with a reduction in dosage towards 0.033 mg/kg/day SC if substantial catch-up growth is seen during the first few years of treatment.
For short stature associated with Turner’s syndrome:
Subcutaneous dosage: Children: Up to 0.067 mg/kg/day SC is recommended.
For short stature in children with Noonan Syndrome:
Subcutaneous dosage: Children: Up to 0.066 mg/kg/day SC is recommended. Prior to initiating somatropin, ensure that the patient has short stature. Not all children with Noonan syndrome have short stature. Twenty-four children aged 3—14 years of age received doses of 0.033 mg/kg/day SC or 0.066 mg/kg/day SC for 2 years; after 2 years, the dose was adjusted based on growth response and continued until final height was achieved. Using the national reference, height gain from baseline increased 1.5 SDS (mean height gain of 9.9 cm in males and 9.1 cm in females at 18 years of age). Using the Noonan reference, height gain from baseline increased 1.6 SDS (mean height gain of 11.5 cm in males and 11 cm in girls at 18 years of age) was noted. During the first 2 years of treatment, height velocity was greater in the group receiving 0.066 mg/kg/day SC.
Maximum Dosage Limits: Somatropin, rh-GH doses must be individualized and are highly variable depending on the nature and severity of the disease, the formulation being used, and on patient response.
Route-Specific Administration:
Injectable Administration: Administer somatropin by intramuscular or subcutaneous injection. Do NOT administer intravenously. Discontinue therapy if final height is achieved or epiphyseal fusion occurs. Visually inspect parenteral products for particulate matter and discoloration prior to administration whenever solution and container permit.
Subcutaneous Administration: Subcutaneous injection of somatropin volumes greater than 1 ml of reconstituted solution is not recommended. Inject SC taking care not to inject intradermally. Allow refrigerated solutions to come to room temperature prior to injection. Subcutaneous injections may be given in the thigh, buttocks, or abdomen. Rotate injection sites daily.
Intramuscular Administration: Inject somatropin deeply into a large muscle. Aspirate prior to injection to avoid injection into a blood vessel. Rotate injection sites daily.
In August 2011, the FDA notified healthcare professionals that it has reviewed data from the SAGhE (Sante Adulte GH Enfant) study (a long-term epidemiological study conducted in France). The SAGhe Study found that patients with idiopathic growth hormone deficiency and idiopathic or gestational short stature treated with somatropin during childhood had a 30% increased risk of death compared to the general population. The FDA determined this evidence regarding recombinant human growth hormone and increased risk of death to be inconclusive. A 2016 study devised an advanced mortality model using the the Swedish Medical Birth Registry to estimate standardized mortality rates in patients receiving growth hormone compared to the general population. The authors concluded that the increase in mortality found in the SAGhE study was most likely related to basic characteristics of the growth hormone deficiency population (i.e. birth weight, birth length, and congenital malformations) rather than due to the use of growth hormone treatment itself.
Somatropin therapy may cause changes in some laboratory values. Serum levels of inorganic phosphorus, alkaline phosphatase, and parathyroid hormone may increase with somatropin therapy.
Somatropin products are contraindicated in patients with a known hypersensitivity to somatropin or any of the product excipients. Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with post-marketing use of somatropin products. Patients and caregivers should be informed that there is a risk of serious hypersensitivity reactions or anaphylaxis and that prompt medical attention should be sought if an allergic reaction occurs. As with any hormonal product, local or systemic allergic reaction may occur. Several of the products contain m-cresol as a preservative. Some of the formulations recommend using sterile water for injection as a diluent in patients with m-cresol hypersensitivity; other products recommend using other formulations. The package insert of the specific product should be consulted for further information when using somatropin in patients with m-cresol hypersensitivity. Similarly, some of the formulations also contain glycerin. Do not use formulations of somatropin that contain glycerin in patients with glycerin hypersensitivity.
Somatropin is contraindicated for growth promotion in pediatric patients with epiphyseal closure. Linear growth can no longer occur in these patients. In addition, slipped capital femoral epiphysis may occur more frequently in patients with endocrine disorders or in patients undergoing rapid growth.
Response to somatropin therapy in children tends to decrease over time. However, in children in whom growth rate is not increased, especially during the first year of treatment, compliance as well as other causes of growth failure including thyroid abnormalities, malnutrition, advanced bone age, and antibodies to somatropin should be assessed. Any child taking somatropin that complains of hip or knee pain or the development of a limp should be evaluated by a clinician. Slipped capital femoral epiphysis may occur more frequently in patients with endocrine disorders or in children undergoing rapid growth. In addition, children with growth failure secondary to renal impairment should be evaluated for progression of renal osteodystrophy. Slipped capital femoral epiphysis or avascular necrosis of the femoral head may occur in children with advanced renal osteodystrophy; x-rays of the hip should occur prior to initiating therapy with somatropin. In August 2011, the FDA notified healthcare professionals that it has reviewed data from the SAGhE (Sante Adulte GH Enfant) study (a long-term epidemiological study conducted in France), which found that patients with idiopathic growth hormone deficiency and idiopathic or gestational short stature treated with somatropin during childhood had a 30% increased risk of death compared to the general population. The FDA has determined the evidence regarding recombinant human growth hormone and increased risk of death to be inconclusive; a number of study design weaknesses were found which limit the interpretability of the study results. Additionally, the FDA reviewed the medical literature, as well as reports from the Agency’s Adverse Event Reporting System (AERS). The FDA will continue to review this safety issue and expects to receive additional data from the SAGhE study in Spring 2012. The FDA will update the public when new information is available. Healthcare professionals and patients should continue to prescribe and use recombinant human growth hormone according to the labeled recommendations.
Some of the multi-dose somatropin products contain benzyl alcohol and should be used cautiously in neonates and patients with benzyl alcohol hypersensitivity. Benzyl alcohol has been associated with toxicity in newborns. If somatropin is to be used in neonates or in patients with benzoyl alcohol hypersensitivity, sterile water for injection, USP should be used for reconstitution and only one dose should be used per vial.
Somatropin is contraindicated in patients with active neoplastic disease. Any pre-existing neoplastic disease, specifically intracranial lesions (including pituitary tumors) must be inactive, and chemotherapy and radiation therapy complete, prior to beginning somatropin therapy. In childhood cancer survivors who were treated with radiation to the brain/head for their first neoplasm and who developed subsequent growth hormone deficiency and were treated with somatropin, an increased risk of a secondary malignancy has been reported. Intracranial tumors, in particular meningiomas, were the most common of these second neoplasms. It is unknown whether there is any relationship between somatropin replacement therapy and CNS tumor recurrence in adults. Monitor all patients with a history of growth hormone deficiency secondary to an intracranial neoplasm routinely while on somatropin therapy for progression or recurrence of the tumor. Because children with certain rare genetic causes of short stature have an increased risk of developing malignancies, consider the risks and benefits of starting somatropin in these patients. If treatment with somatropin is initiated, these patients should be carefully monitored for development of neoplasms. Monitor patients on somatropin therapy carefully for increased growth, or potential malignant changes, of preexisting nevi. Somatropin therapy should be discontinued if evidence of neoplasia develops.
Somatropin is contraindicated in patients with acute critical illness due to complications following open heart or abdominal surgery, multiple accidental trauma or to patients having acute respiratory insufficiency. Two placebo-controlled clinical trials in non-growth hormone deficient adult patients (n=522) with these conditions revealed a significant increase in mortality (41.9% vs. 19.3%) among somatropin-treated patients (5.3—8 mg/day) compared to those receiving placebo. The safety of continuing somatropin treatment in patients receiving replacement doses for approved indications who currently develop these illnesses has not been established. Therefore, the potential benefit of treatment continuation with somatropin in patients having acute critical illnesses should be weighed against the potential risk. Additionally, somatropin is contraindicated for use in pediatric patients with Prader-Willi syndrome and respiratory insufficiency as there have been reports of fatalities (see Prader-Willi discussion).
The manufacturers of Genotropin and Norditropin indicate that adult patients with obesity receiving somatropin for growth hormone deficiency may be more likely to experience adverse events when dosed by weight (see Dosage). Using a daily dose that is not weight-based may be preferable. Additionally, somatropin is contraindicated for use in pediatric patients with Prader-Willi syndrome and obesity as there have been reports of fatalities (see Prader-Willi discussion).
Somatropin is contraindicated in patients with Prader-Willi syndrome who are severely obese or have severe respiratory impairment. Unless patients with Prader-Willi syndrome also have a diagnosis of growth hormone deficiency, somatotropin is not indicated for long-term treatment of pediatric patients who have growth failure due to genetically confirmed Prader-Willi syndrome. There have been reports of fatalities with the use of growth hormone in pediatric patients with Prader-Willi syndrome who had one or more of the following risk factors: severe obesity, history of respiratory insufficiency or sleep apnea, or unidentified respiratory infection. Male patients with one or more of these factors may be at increased risk. Patients with Prader-Willi syndrome should be evaluated for upper airway obstruction before initiation of treatment with growth hormone. If during treatment with growth hormone patients show signs of upper airway obstruction (including onset of or increased snoring), treatment should be interrupted. All patients with Prader-Willi syndrome should be evaluated for sleep apnea and monitored if sleep apnea is suspected. All patients with Prader-Willi syndrome should also have effective weight control and be monitored for signs of respiratory infections, which should be diagnosed as early as possible and treated aggressively. Patients with Prader-Willi syndrome may also be at increased risk of intracranial hypertension.
Somatropin should be used cautiously in patients with diabetes mellitus. Patients with diabetes or glucose intolerance and those patients with risk factors for diabetes or glucose intolerance should be monitored closely during treatment with somatropin. Risk factors for glucose intolerance include obesity (including obese patients with Prader-Willi Syndrome), Turner syndrome, or a family history of type II diabetes. Because somatropin may reduce insulin sensitivity, especially at higher doses, patients should be monitored for evidence of glucose intolerance. Glucose intolerance or acromegaly may occur with chronic overdosage of somatropin. Dose adjustments of antidiabetic medications may be necessary when somatropin is initiated. Due to the effects of somatropin on insulin sensitivity and blood glucose concentrations, somatropin is contraindicated in patients with diabetic retinopathy.
Patients with a history of scoliosis should receive somatropin with caution. Because growth hormone increases growth rate, patients with scoliosis can experience progression of scoliosis. Patients should be monitored for progression of scoliosis. In addition, skeletal abnormalities including scoliosis are commonly seen in untreated Turner’s syndrome, Noonan’s syndrome, and Prader-Willi syndrome patients. Clinicians should be aware of these abnormalities, which may manifest during growth hormone therapy.
Patients who have or at risk for pituitary hormone deficiencies, and are receiving somatropin, may be at risk for reduced serum cortisol levels and/or unmasking of central (secondary) adrenal insufficiency. Patients treated with glucocorticoid replacement for previously diagnosed adrenal insufficiency may require an increase in their maintenance or stress doses following initiation of somatropin treatment. In addition, patients with untreated hypothyroidism will have an inadequate response to somatropin therapy. Changes in thyroid hormone plasma levels may develop during somatropin therapy because patients with Turner’s syndrome have an inherent risk of developing autoimmune thyroid disease. Periodic thyroid function tests should be performed and treatment with thyroid hormone initiated when indicated.
Somatropin therapy has been reported to cause increased intracranial pressure with papilledema, visual changes, headache, and nausea and/or vomiting. Symptoms usually occurred within the first eight weeks of somatropin therapy. Resolution of intracranial hypertension-associated symptoms occurred after discontinuation of somatropin therapy or after a reduction in the hormone dose. Funduscopic examination is recommended at the initiation and periodically during the course of somatropin therapy. Patients with chronic renal insufficiency, Prader-Willi syndrome, and Turner’s syndrome may be at increased risk for developing intracranial hypertension.
No adequate and well controlled studies have been conducted in pregnant humans, and the potential for somatropin to cause adverse effects on the fetus or reproductive system is unknown. In animal studies that have been performed, differing doses exceeding the regular human dose revealed no evidence of impaired fertility or harm to the fetus. Inform females of childbearing age that use of somatropin during pregnancy has not been studied in humans, therefore, the effects of the drug on the fetus are unknown.
No data are available regarding the presence of somatropin in human milk, the effects of somatropin on the breast-fed infant, or the effects of somatropin on milk production. Limited published literature reports no adverse effects on breast-feeding infants with maternal administration of somatropin and no decrease in milk production or change in milk content during treatment with somatropin. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally administered drug, healthcare providers are encouraged to report the adverse effect to the FDA.
During treatment with somatropin, Turner’s syndrome patients should be evaluated carefully for otitis media and other ear disorders since these patients have an increased risk of ear or hearing disorders. In addition, patients with Turner’s syndrome should be monitored closely for cardiovascular disorders such as stroke, aortic aneurysm, and hypertension because these patients are also at risk for these conditions.
Clinical studies of somatropin did not include sufficient numbers of geriatric subjects; however, reported clinical experience has not identified differences in responses between geriatric and younger adult patients. In general, dose selection for an older adult should be cautious, usually starting at the low end of the dosing range. Geriatric patients are more at risk for the adverse effects of therapy compared to pediatric and younger adult patients. According to practice guidelines, growth hormone/somatropin should only be prescribed to patients with clinical features suggestive of adult growth hormone deficiency (GHD) and biochemically proven evidence of adult GHD. There are no data are available to suggest that somatropin has beneficial effects in treating aging and age-related conditions and the enhancement of sporting performance; therefore, the prescription of the drug to adult patients for any reason other than the well-defined approved uses of the drug is not recommended. According to the Beers Criteria, growth hormone is considered a potentially inappropriate medication (PIM) for use in geriatric patients and should be avoided due to its small effect on body composition relative to a significant adverse effect profile (e.g., edema, arthralgia, carpal tunnel syndrome, gynecomastia, elevated fasting glucose). However, the Beers expert panel considers hormone replacement after pituitary gland removal to be an acceptable use in the elderly.
Somatropin (Serostim) has been used in patients with HIV-associated adipose redistribution syndrome (HARS); somatropin therapy may be less effective in females with HARS as compared to men. During clinical trials, 47 women receiving somatropin showed no difference from placebo with respect to reduction in visceral adipose tissue (VAT). Reasons for the lack of effectiveness may be the concomitant use of estrogen (6 patients) or a lower baseline VAT level as compared to men. Lower VAT levels have been demonstrated in several clinical trials to be associated with a reduced response to somatropin.
Patients who develop persistent, severe abdominal pain during somatropin treatment should be evaluated for pancreatitis, especially pediatric patients. Use with caution in patients with a past history of pancreatitis or with risk factors for pancreatitis. Pancreatitis has been rarely reported in adults and children receiving somatropin, with pediatric patients appearing to be at greater risk compared to adults. Girls with Turner syndrome may have an even greater risk of developing pancreatitis compared to others undergoing somatropin treatment.
No adequate and well controlled studies have been conducted in pregnant humans, and the potential for somatropin to cause adverse effects on the fetus or reproductive system is unknown. In animal studies that have been performed, differing doses exceeding the regular human dose revealed no evidence of impaired fertility or harm to the fetus. Inform females of childbearing age that use of somatropin during pregnancy has not been studied in humans, therefore, the effects of the drug on the fetus are unknown.
No data is available regarding the presence of somatropin in human milk, the effects of somatropin on the breast-fed infant, or the effects of somatropin on milk production. Limited published literature reports no adverse effects on breastfeeding infants with maternal administration of somatropin and no decrease in milk production or change in milk content during treatment with somatropin. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally administered drug, healthcare providers are encouraged to report the adverse effect to the FDA.
The effects of somatropin (Humatrope) on bone mineral density (BMD) and bone mineral content (BMC) have been evaluated in patients with adult-onset growth hormone deficiency and adults with childhood-onset GH deficiency still requiring somatropin therapy as adults (transition patients). Men, but not women, in the adult-onset study had an increase of 4% in lumbar spine BMD relative to placebo. No significant change in hip BMD was seen in women or men. In transition patients, patients randomized to 12.5 mcg/kg/day of somatropin, versus 25 mcg/kg/day or placebo, experienced an increase of 2.9% in total BMC; patients in the other two groups did not experience any changes. Increases in lumbar spine BMD and BMC were also statistically significant in the 12.5 mcg/kg/day treatment group. The occurrence of osteoporotic fracture was not studied.
The effect of somatropin (Nutropin AQ) on visceral adipose tissue has been evaluated in an open-label trial of adult patients with both childhood-onset and adult-onset GH deficiency. Doses of somatropin of up to 0.012 mg/kg per day in women (all of whom received estrogen replacement therapy) and men under age 35 years, and up to 0.006 mg/kg per day in men over age 35 years were administered for 32 weeks. Compared with untreated patients, after 32 weeks visceral adipose tissue (VAT) in patients treated with somatropin decreased by 14.2% (p = 0.012). The effect of reducing VAT in adult GHD patients with somatropin on long-term cardiovascular morbidity and mortality has not been determined.
Somatropin has been associated with an increased risk of a secondary malignancy. Leukemia has been reported in a small number of growth hormone deficient patients treated with somatropin. It is uncertain if this increased risk is related to the pathology of growth hormone deficiency itself, growth hormone therapy, or other associated treatments such as radiation therapy for intracranial tumors. Additionally, in childhood cancer survivors who were treated with radiation to the brain/head for their first neoplasm and who developed subsequent growth hormone deficiency and were treated with somatropin, an increased risk of a secondary malignancy has been reported. Intracranial tumors, in particular meningiomas, were the most common of these second neoplasms. It is unknown whether there is any relationship between somatropin replacement therapy and CNS tumor recurrence in adults. Monitor all patients with a history of growth hormone deficiency secondary to an intracranial neoplasm routinely while on somatropin therapy for progression or recurrence of the tumor. Because children with certain rare genetic causes of short stature have an increased risk of developing malignancies, consider the risks and benefits of starting somatropin in these patients. If treatment with somatropin is initiated, these patients should be carefully monitored for development of neoplasms. Monitor patients on somatropin therapy carefully for increased growth, or potential malignant changes, of preexisting nevi. Somatropin therapy should be discontinued if evidence of neoplasia develops.
In trials of growth hormone deficient (GHD) adults, rates of edema or peripheral edema have varied according to the brand of somatropin used and ranged from approximately 5% to 45%. In children with GHD, the rates have been approximately 3%. The edema appears to occur early in therapy and may be transient and/or respond to a dose reduction. Both fluid retention and peripheral edema have been commonly reported in patients receiving somatropin. Peripheral edema is more common in adults than children.
Increased intracranial pressure (intracranial hypertension), with papilledema, visual changes, severe head pain, nausea, and vomiting, has been reported in a small number of patients treated with growth hormone products. Symptoms usually occur within the first 8 weeks of treatment initiation. In all reported cases, symptoms resolved after termination of therapy or a reduction in dose. Funduscopic examination of patients is recommended upon initiation of therapy and periodically throughout treatment. If papilledema is observed during treatment, somatropin should be stopped. If intracranial hypertension is diagnosed, the treatment can be restarted at a lower dose. Patients with Turner syndrome may also be at an increased risk for developing intracranial hypertension.
Joint swelling (5—6%), myalgia (3—30%), musculoskeletal pain (5—14%), pain and stiffness of the extremities (2—19%), and back pain (3—11%) have been commonly associated with somatropin therapy. Some events are related to fluid retention and appear to occur more frequently in adults than in children, particularly arthralgia (11—37%). In adults treated with somatropin, muscle and joint pain usually occurred early in therapy and tended to be transient or respond to dosage reduction. Pain, swelling and/or stiffness may resolve with analgesic use or a reduction in frequency of dosing with somatropin. In addition, carpal tunnel syndrome (nerve entrapment syndrome, 1—5%) and arthrosis (8—11%), have also been reported. More serious adverse reactions that have been reported include slipped capital femoral epiphysis and progression of scoliosis (4—19%) in pediatric patients.
Metabolic complications have been frequently reported with somatropin therapy. During post-marketing surveillance of various products, there have been cases of new onset glucose intolerance, hyperglycemia, diabetes mellitus, and exacerbation of pre-existing diabetes mellitus. Some patients developed diabetic ketoacidosis and diabetic coma. Discontinuing treatment led to improvement in some patients, while glucose intolerance persisted in others. Monitor glucose concentrations closely during therapy; initiate or adjust antidiabetic treatment as necessary. Short-term overdosage may result in hypoglycemia. A greater incidence of impaired glucose tolerance has been observed with higher doses. In patients with Turner syndrome treated with Norditropin, impaired fasting glucose after 4 years of treatment occurred in 22% of patients receiving 0.045 mg/kg/day for 1 year followed by 0.067 mg/kg/day thereafter compared with 5% of patients receiving 0.045 mg/kg/day. Hypothyroidism has been reported in approximately 5—16% of patients receiving somatropin therapy. During a 6 month placebo-controlled trial in growth hormone deficient (GHD) adults using the Saizen brand, approximately 10% required small upward adjustments of thyroid hormone replacement therapy for preexisting hypothyroidism, and 1 patient was newly diagnosed with hypothyroidism. Additionally, during the trial, 2 patients required upward adjustments of hydrocortisone maintenance therapy (unrelated to intercurrent stress, surgery, or disease) for preexisting hypoadrenalism, and 1 patient was newly diagnosed with adrenal insufficiency. Monitor thyroid tests periodically and initiate or adjust thyroid replacement therapy as necessary. Hyperlipidemia (8%) has also been reported, most often as hypertriglyceridemia (1—5%).
The most common central nervous system (CNS) adverse reactions reported in somatropin clinical trials were in adults and include headache (6—18%), paresthesias (2—17%), and hypoesthesia (2—15%). Asthenia or weakness (3—6%), fatigue (4—9%), insomnia (5%), depression (5%) and dizziness were also reported in trials. Seizures have been reported rarely.
Flu like symptoms have been reported in approximately 4—23% of somatropin-treated patients in clinical trials. Upper respiratory tract infection (e.g., naso-pharyngitis 3—14%, bronchitis 9%, and rhinitis 6—14%) has been reported at a similar frequency. Children with Turner syndrome reported otitis media (16—43%) and ear disorders (18%). In a study with Norditropin, patients in group 1 (0.045 mg/kg/day for year 1, 0.067 mg/kg/day for year 2, and 0.089 mg/kg/day thereafter) experienced a higher rate of otitis media of 86.4% compared to 78.3% of patients in group 2 (0.045 mg/kg/day for 1 year followed by 0.067 mg/kg/day thereafter) and 69.6% of patients in group 3 (0.045 mg/kg/day). These findings suggest higher doses may increase the risk of otitis media, and it should be noted that 40—50% of the cases were considered to be serious. Increased cough (6%) has also been reported.
Somatropin administration is associated with an injection site reaction (pain or burning associated with injection), lipoatrophy, or nodule formation; lipoatrophy can be avoided by frequent rotation of the injection site. Other injection site reactions include hematoma (9%), fibrosis, erythema, pruritus, rash, swelling, bleeding, and skin hyperpigmentation.
Antibody formation occurs in approximately 2% of patients receiving somatropin. Growth hormone antibody binding capacities below 2 mg/L have not been associated with growth attenuation; however, in some cases when binding capacity exceeds 2 mg/L growth attenuation has been observed. Testing for growth hormone antibodies should be performed in any patient who fails to respond to somatropin therapy.
During post-marketing experience with somatropin, dermatologic and serious systemic hypersensitivity reactions including anaphylactoid reactions and angioedema have been reported. Acne vulgaris (6%), diaphoresis (8%), alopecia, and eczema have been reported in patients taking somatropin therapy. Allergic reactions are possible and include rash (unspecified), and exacerbation of pre-existing psoriasis has been reported.
Pancreatitis has been rarely reported in adults and children receiving somatropin, with children, and especially girls with Turner syndrome, appearing to be at greater risk compared to adults. Evaluate any patient who develops abdominal pain for pancreatitis. Other gastrointestinal adverse reactions reported in clinical trials include elevated hepatic enzymes (6—13%), gastritis (6%), and gastroenteritis (8%).
Gynecomastia has been observed in both adults (3—6%) and children (5—8%) treated with somatropin in clinical trials.
Hypertension (3—8%) and chest pain (unspecified) (5%) have been reported in patients treated with somatropin in clinical trials. Eosinophilia was reported in approximately 12% of pediatric patients receiving somatropin in clinical trials. Hematuria has been rarely observed.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
1.Omnitrope (somatropin) package insert. Princeton, NJ: Sandoz, Inc.; 2016 Dec.
2.Genotropin (somatropin) package insert. New York, NY: Pharmacia & Upjohn Company; 2016 Dec.
3.Food and Drug Administration (US FDA) Drug Safety Communication. Safety review update of Recombinant Human Growth Hormone (somatropin) and possible increased risk of death. Retrieved August 4, 2011. Available on the WorldWide Web at: http://www.f
4.Albertsson-Wikland K, Martensson A, Savendalh L, et al. Mortality is not increased in recombinant human growth hormone-treated patients when adjusting for birth characteristics. J Clin Endocrinol Metab. 2016; 101: 2149-2159.
5.Humatrope (somatropin) package insert. Indianapolis, IN: Eli Lilly and Company; 2016 Dec.
6.Serostim (somatropin) package insert. Rockland, MA: EMD Serono, Inc.; 2017 May.
7.Nutropin (somatropin) package insert. San Francisco, CA: Genentech; 2016 Dec.
8.Accretropin (somatropin) package insert. Winnipeg, Canada: Cangene Corporation; 2016 Dec.
9.Nutropin AQ (somatropin) package insert. San Francisco, CA: Genentech; 2016 Dec.
10.Saizen (somatropin) package insert. Rockland, MA: EMD Serono Inc; 2017 May.
11.Norditropin (somatropin) package insert. Plainsboro, NJ: Novo Nordisk; 2016 Dec.
12.Zomacton (somatropin) package insert. Parsippany, NJ: Ferring Pharmaceuticals, Inc; 2016 Dec.
13.Zorbtive (somatropin) injection package insert. Rockland, MA: EMD Serono, Inc.; 2017 May.
14.Cook DM, Yuen KC, Biller BM, et al; American Association of Clinical Endocrinologists (AACE). American Association of Clinical Endocrinologists medical guidelines for clinical practice for growth hormone use in growth hormone-deficient adults and
15.The American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2015;63:2227-46.
Be the first to review “Zomacton Injection”
General Inquiries
There are no inquiries yet.









Reviews
There are no reviews yet.