- Description
- Reviews (0)
- Store Policies
- Inquiries
Description
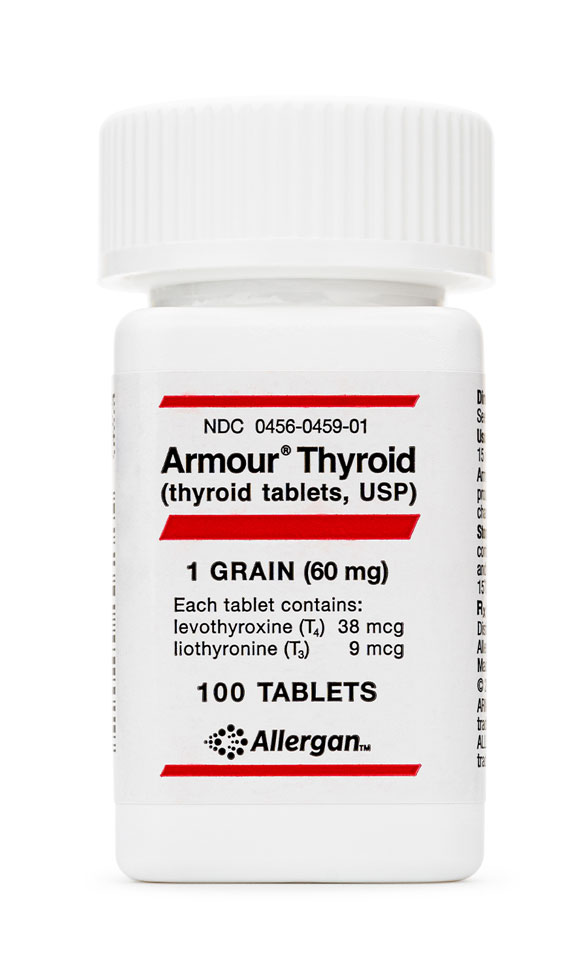
Dosage Strengths of Thyroid (Desiccated Porcine) Capsules
Immediate Release: 15 mg, 30 mg, 45mg, 60 mg, 75 mg, 90 mg, 120 mg, 150 mg, 180 mg
Slow Release: 15 mg, 30 mg, 45mg, 60 mg, 75 mg, 90 mg, 120 mg, 150 mg, 180 mg
Located in the front of the neck in the human body, the thyroid gland is an endocrine gland responsible for the production of the thyroid hormones triiodothyronine (T3) and tetraiodothyronine, also known as thyroxine (T4). The thyroid hormone exerts its effects throughout the entire body; it plays an essential role in metabolism, bone growth, as well as many other processes and functions within the body. Most of the regulatory and metabolic actions of thyroid hormones are carried out by T3, which is the active form. T4 is mostly inactive and has to be converted in to active T3 before it can exert it effects in the body.
Unlike most other hormones, the effects of the thyroid hormone are widespread throughout the entire body and not limited to a single organ or body system. Some effects of thyroid hormone include:
- Cardiovascular system: Thyroid hormones causes and increase in the expression of beta-receptors in the body. This increased expression has positive chronotropic and inotropic effects of the cardiac muscles resulting in an increased cardiac output, stroke volume, and resting heart rate. There is also an increased inotropic effect as thyroid hormone causes an increase in intracellular calcium within the myocardium. Additionally, thyroid hormones cause a decrease in peripheral vascular resistance through the dilatation of the cardiac, skin, and muscle vessels. Furthermore, thyroid hormones activate the renin-angiotensin-aldosterone system which results in an increased blood volume due to an increase in fluid reabsorption.
- Respiratory system: T3 enhances the production of erythropoietin and hemoglobin which thereby increases the amount of oxygen delivered to the body tissues. It enhances the production of erythrocytes by improving folate and cobalamin absorption from the gastrointestinal tract; this allows for an increased capacity in oxygen delivery to tissues. The active thyroid hormone also stimulates resting respiratory rate as well as minute ventilation in instances of increased oxidation to ensure that blood oxygen levels remain within its normal range.
- Metabolism: T3 is directly responsible for the basal metabolic rate (BMR) and heat production (thermogenesis) in the body. Increased T3 levels results in an increased BMR as well as thermogenesis which is the pathogenesis behind the excessive sweating associated with hyperthyroidism. It also stimulates carbohydrate catabolism, protein anabolism, as well as lipid synthesis.
- Neurological system: Within the peripheral nervous system, T3 promotes an increase in peripheral reflexes and gastrointestinal motility; the increased reflexes is also due to the effect of T3 on increasing the production of Type II (fast twitch) muscle fibers. Additionally, T3 helps in increased alertness and responsiveness to the external environment. Furthermore, T3 is important in brain development because it stimulates the growth of axons within the neuron and myelin sheath formation.
- Skeletal system: Within the maternal uterus, T3 is key in the developing fetal growth centers. In children, T3 is needed for linear bone growth, endochondral ossification and maturation of the epiphyseal bone centers. T3 deficiency in childhood may result in stunting of bone growth and development; this may become permanent even after the administration of supplemental thyroid hormone.
- Reproductive system: T3 plays an essential role in the reproductive health in both men and women the regulation of the regulatory cycle and spermatogenesis respectively.
Given the wide-ranging roles of thyroid hormone in the human body, it is essential that its levels are well-maintained within the recommended range. Generally, normal levels of T3 should fall between 100 – 200 ng/dL, depending on the age and gender of the individual. When serum T3 levels fall below the recommended range, a condition known as hypothyroidism, oral thyroid supplementation may be warranted to prevent the disruption of systems and processes dependent on this hormone.
The synthesis of thyroid hormones T3 and T4 begin with the production and release of the tripeptide Thyrotropin Releasing Hormone (TRH) from the paraventricular nucleus of the hypothalamus within the brain. The released TRH is then transported to the anterior pituitary gland by means of the portal capillary plexus where it stimulates the production and release of Thyroid Stimulating Hormone (TSH) from the thyrotroph cells. Subsequently, TSH stimulates thyroid follicular cells on the thyroid gland to effectuate the release of T4 which is then converted into the more potent hormone T3. The conversion on T4 into T3 is mediated by the enzymes deiodinases I and II; these enzymes work by catalyzing the removal of a 5′-iodine atom from T4. Type I deiodinase is located mainly in peripheral organs such as kidney or liver and is the site for most of the conversion of T4 to T3. Type II deiodinase is found mainly in the brain and adipose tissue where it performs functions similar to Type I deiodinases.
Thyroid hormones exert their effects on the different tissues and organs of the body by means of two types of thyroid receptors namely Thyroid Receptor (TR) alpha and TR-beta. TR-alpha and TR-beta both perform similar roles by enabling the action of thyroid hormones on the target cells, but they have different patterns of expression in different tissues within the body. TR-alpha is expressed mostly in the heart, brain, skeletal muscle, and bone while TR-beta is expressed in the liver, pituitary, and hypothalamus.
Once produced and released, the thyroid hormones enter into the nucleus of the target cells where it then proceeds to bind with either TR-alpha or TR-beta, depending on the cell. Once bound, the complex then causes changes within the cell through genetic transcription, synthesis of messenger RNA, as well as cytoplasmic protein production. These genomic changes are responsible for most of the effects of thyroid hormones on target tissues.
In addition to its genomic actions, several studies have demonstrated that thyroid hormones also exert their effects on target tissues through non-genomic pathways. In the non-genomic pathway, thyroid hormones interact with the receptor Avb3 at the plasma membrane. This interaction results in the activation of mitogen-activated protein kinase, otherwise known as ERK1/2, when then modulates ion transport systems or cellular proliferation.
There are several factors that should be taken into consideration prior to the administration of exogenous thyroid hormones. Some of these factors are an absolute contraindication to thyroid hormone administration while for others, close and careful monitoring may be required. These factors include:
- Hypersensitivity: Extreme care should be taken when administering thyroid hormones to individuals who have demonstrable hypersensitivity to the hormone or other components in the preparation.
- Adrenal insufficiency: Thyroid hormone replacement is contraindicated in individuals with untreated adrenal insufficiency as this may provoke an acute adrenal crisis.
- Cardiovascular disease: Due to the cardio stimulatory effects of thyroid hormones, care should be exercised when initiating thyroid replacement therapy in individuals with cardiac diseases such as angina, arrhythmias, or a previous myocardial infarction.
- Diabetes: Thyroid hormone therapy can disrupt blood sugar levels in diabetics such that an adjustment of the diabetic medications may be warranted.
- Renal disease: Since T3 and T4 are primarily excreted by the kidneys, care should be taken to prevent toxicity when thyroid hormones are administered to individuals with any degree of renal impairment.
- Gastrointestinal disorders: GI disorders such as celiac disease and Helicobacter pylori can cause compromise the intestinal tract and impair the absorption of orally ingested thyroid hormone.
There have been no reported major birth defects or miscarriages in women receiving thyroid hormone replacement during pregnancy. Thyroid hormone replacement is indicated in pregnancy if the need arises because hypothyroidism in pregnancy is a greater threat to both mother and fetus.
Exogenous thyroid hormones is also expressed in breast milk, however, studies conducted have not reported any adverse effects in nursing infants.
Thyroid hormone replacement is generally well tolerated in individuals. However, some individuals may develop mild side effects such as nausea, diarrhea, fatigue, flushing, and irritability, among others. In some instances, individuals may develop more serious reactions such as atrial fibrillation, seizures, cardiac arrest, and thyrotoxicosis; development of these serious adverse reactions require prompt medical intervention.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
1.Armstrong, M., Asuka, E., Fingeret, A., “Physiology, Thyroid Function”, StatPearls. Treasure Island (FL). Available: https://www.ncbi.nlm.nih.gov/books/NBK537039/
2.Shahid, M.A., Ashraf, M.A., Sharma, S., “Physiology, Thyroid Hormone”, “, StatPearls. Treasure Island (FL). Available: https://www.ncbi.nlm.nih.gov/books/NBK500006/
3.Williams, G.R., “Thyroid Hormone Actions in Cartilage and Bone”, European Thyroid Journal, vol.2 issue 1, pp. 3-13. 2012. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821494/
4.Basile, L.,M., “What are T3, T4, and TSH?”, Endocrine Web. Available: https://www.endocrineweb.com/thyroid-what-are-t3-t4-tsh
5.Mohan, S., Kim, H., “Role and Mechanisms of Action of Thyroid Hormone on the Skeletal Development”, Bone Research, vol.1, pp. 146 – 161. Available: https://www.nature.com/articles/boneres201311
6.Yen, P.,M., “Physiological and Molecular Basis of Thyroid Hormone Action”, Physiological Reviews, vol.81 issue 3, pp. 1097 – 1142. 2001. Available: https://journals.physiology.org/doi/full/10.1152/physrev.2001.81.3.1097
7.Brent, G.,A., “Mechanisms of thyroid hormone action”, Journal of Clinical Investigation, vol.122, issue 9, pp. 3035-3043. 2012. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3433956/
8.”Levothyroxine”, Drug Bank. Available: https://go.drugbank.com/drugs/DB00451
9.Colucci, P., Yue, S.C., Ducharme, M., Benvenga, S., “A Review of the Pharmacokinetics of Levothyroxine for the Treatment of Hypothyroidism”, European Endocrinology, vol.9 issue 1, pp. 40-47. 2013. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6193522/
12.”Levothyroxine sodium – Drug Summary”, Prescribers Digital Reference. Available: https://www.pdr.net/drug-summary/Levothyroxine-Sodium-Injection-levothyroxine-sodium-3865
13.”Levothyroxine Pregnancy and Breastfeeding Warnings”. Available: https://www.drugs.com/pregnancy/levothyroxine.html
Be the first to review “Thyroid Desiccated Porcine Capsules”
General Inquiries
There are no inquiries yet.









Reviews
There are no reviews yet.